Norman J. Strupp Professor of Neurology; Head, Cerebrovascular Disease; Section, Department of Neurology; Director, Hope Center Animal Surgery Core; Co-Director, Stroke and Cerebrovascular Center
Research Interests
Our lab is interested in several exciting research projects spanning in vitro studies in cell culture, in vivo studies in animal models of disease, and clinical studies using data from human patients.
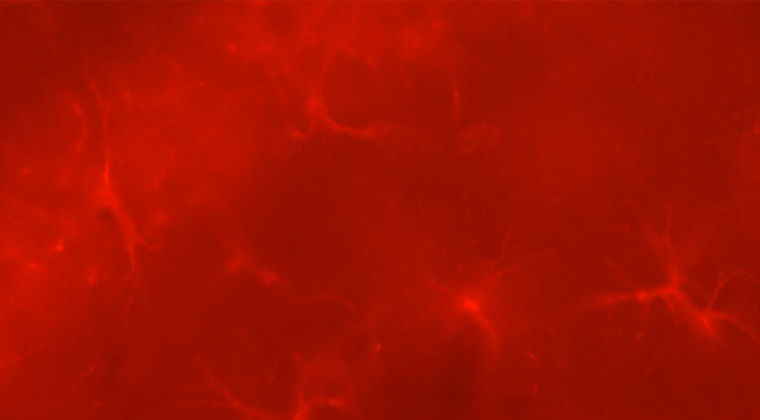
- Cellular Processing of APP in Alzheimer’s Disease (AD): AD is characterized by the deposition of extracellular plaques comprised of primarily of the amyloid beta peptide (Aβ), a peptide derived from serial proteolytic cleavages of the Amyloid Precursor Protein (APP). We study the cellular and molecular mechanisms of Aβ generation, aggregation, clearance, and deposition as plaques. In particular, we have developed a novel technique using fluorogenic click chemistry and advanced microscopy techniques in live cells to visualize APP proteolysis and subsequent Aβ generation, and their respective trafficking itineraries. We hypothesize that the earliest aggregates of Aβ form intracellularly in the endosome-lysosome system, prior to plaque development.
- Neuroplasticity after stroke: Ischemic stroke is a leading cause of disability that directly damages the circuitry of the brain. There is a great need for precision medical therapies to increase plasticity and recovery in human patients. We use mouse models of stroke to study the central mechanisms underlying plasticity in the brain after injury, and how they can be targeted with gene therapy. We collaborate with several groups in the Radiology department and use novel optical neuroimaging techniques and electrophysiology to measure the connectivity of brain networks and how they are affected by injury and therapy.
- Genetic influences on early outcomes after acute ischemic stroke: We use genome-wide-association studies to identify genetic variants, genes, and pathways implicated in brain injury mechanisms after acute ischemic stroke. Using a variety of phenotypes, including clinical and neuroimaging quantitative endophenotypes, we are interested in understanding the underlying genetic architecture of primary and secondary brain injury. By finding genetic loci associated with these phenotypes, we hope to identify potential targets for therapeutic intervention to attenuate brain injury after ischemia.
- Pathophysiology of Cerebral Small Vessel Disease and Vascular Dementia: Using advanced MR imaging, we are measuring cerebral blood flow (CBF) and oxygen metabolism in young and aged subjects with and without cerebral small vessel disease (CSVD). We are testing the hypothesis that white matter hyperintensities (WMHs) are caused by chronic ischemia due to CSVD, and that the precise spatial pattern of WMHs may indicate different underlying CSVDs.
Professional Education
- BA: 1985 Yale University, New Haven, Connecticut
- MD: 1993 Cornell University Medical College, New York, New York
- Residency: 1997 Hospital of the University of Pennsylvania, Philadelphia, Pennsylvania
- Fellowship: 1999 Cerebrovascular, Washington University School of Medicine/Barnes-Jewish Hospital, St. Louis, MO
Affiliations
- Neurology
- Adult Neurology
- Hope Center for Neurological Disorders
- Stroke and Cerebrovascular Center
- Bursky Center for Human Immunology & Immunotheraphy Programs (CHiiPs)
- Biology and Biomedical Sciences
- Institute of Clinical and Translational Sciences
Lee Lab
We are engaged in translational research to investigate cellular and molecular mechanisms involved in acute and chronic brain injury, with a focus on Ischemic stroke and Alzheimer’s disease.
